Being ready for the Unexpected – Jim Howson focuses on Clinical Center emergency preparedness

Tucked away on the 6th floor of the NIH Clinical Center is a man who spends all day thinking about what can go wrong. Jim Howson, the hospital's Emergency Coordinator, coordinates and plans responses to possible disaster scenarios that could occur at the Clinical Center.
"I look at what can go wrong and how can we keep it from going wrong," said Howson. Upon his arrival to the Clinical Center in 2018, he said, "The thing that impressed me most is how the staff takes care of patients, and if something does go wrong, how committed staff are to making sure that it doesn't happen again."
Emergency management at NIH has evolved over the years. After the 9/11 attacks, emergency planning at the Clinical Center focused on caring for overflow patients from Suburban Hospital and Walter Reed in the case of a mass casualty event. More recently, the Clinical Center has pivoted to a new role: providing specialists to be resources for the other hospitals in the case of an emergency. The Clinical Center and the NIH are uniquely able to tap into specialized expertise on specific emergencies like Ebola virus exposure.
"This role makes more sense for us as we're less likely to take in patients since the Clinical Center doesn't have an emergency room and isn't used to taking patients off the street," said Howson.
In addition to reviewing the hospital emergency policies and approaches, Howson sees effective communication as one of his major responsibilities. "9/11 was a big motivator to think about disasters, but we're almost 20 years on, what can we improve? How do we let people know we're in an emergency situation and improve our communication in getting the message out?" he asks.
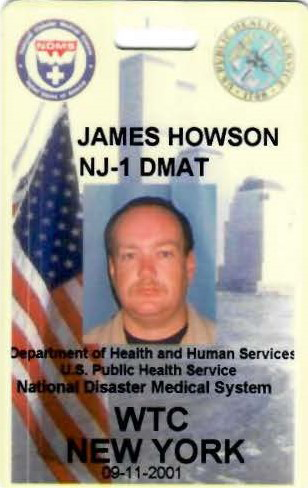
Howson came to the NIH with a breadth of experience. He served as a member of the National Disaster Medical System (NDMS), a partnership of the U.S. Departments of Health and Human Services, Homeland Security, Defense and Veterans Affairs. Through his work in the NDMS, he helped mobilize field hospitals under Disaster Medical Assistance Teams, which were usually deployed in response to natural disasters.
On the morning of Sept. 11, 2001, Howson was called within an hour of the planes hitting the twin towers. His focus was on treating the injuries of rescue workers and supporting the recovery work focused on retrieving remains from the wreckage.
After 9/11, Howson worked for the New Jersey Hospital Association developing education and training programs focused on disaster management. Then he moved on to Booz Allen Hamilton where he traveled the country working with Veterans Administration medical centers to hit baseline requirements on their disaster preparedness planning.
He later moved to U.S. State Department to provide tactical paramedic instruction. The job quickly evolved as Howson focused on training embassy staff how to provide emergency first aid, and then was consulted on the design and planning of U.S. embassies to keep the embassy and staff safe.
In late spring, Howson and the NIH Clinical Center were ready for an unannounced emergency management simulation – a derecho storm that could douse the NIH campus with inches of rain over the course of several hours and high winds that had the potential to blow out windows, damage labs and severely impact the operations of the hospital.
This time around, staff and patients weren't soaked – it was all a part of a Code Yellow exercise undertaken by the Clinical Center's leadership.
A Code Yellow is any type of disaster or potentially harmful event that affects the Clinical Center. It's an occurrence that the Clinical Center hopes not to experience, including severe weather events, pipe breakages and power outages. But when these happen, the command staff is activated to respond.
Howson says he even feels that failures during simulations are instructive, because they provide examples of where systems break down and indicate how things can be improved.
This Code Yellow exercise was a partial surprise, but hospital leaders didn't want it to disrupt patient care, so staff were given a general indication that something was coming but were not provided with any specifics.
The Code Yellow simulation for the derecho was planned as a joint exercise with three months of regional preparation. Montgomery County, Md., ran the exercise along with Walter Reed Military, the National Military Medical Center, with the Clinical Center joining in to help practice its planning skills, to strengthen ties with the community and to maintain the Clinical Center's role as an international, national and regional resource.
The Joint Commission (the independent, not-for-profit organization that accredits and certifies nearly 21,000 health care organizations and programs in the United States), recommends that health care facilities host two emergency exercises a year.
- Robert Burleson and Donovan Kuehn