Ribbon-cutting, open house introduce new Metabolic Clinical Research Unit
 |
(left to right) Terri Wakefield, director of clinical research services for core intramural NIDDK; Acting NIDDK Director Dr. Griffin Rodgers; CC Director Dr. John I. Gallin; Dr. Marvin Gershengorn, NIDDK intramural research scientific director; Dr. Monica Skarulis, senior clinical investigator with NIDDK’s Clinical Endocrine Branch; Dr. Michael Gottesman, NIH deputy director for intramural research; NIH Director Dr. Elias Zerhouni; and Lorie Purdie, nurse manager for the CC’s inpatient services division, open the unit.
|
The new NIH Metabolic Clinical Research Unit, which houses specialized, state-of-the-art facilities for comprehensive research on factors driving obesity, opened to Clinical Center and NIH staff following a ribbon-cutting ceremony on Jan 25. The CC and NIDDK worked closely together to develop the unit. An important component of the NIH Strategic Plan for Obesity Research, the unit and work conducted there will help generate new knowledge regarding the physiology, prevention, and treatment of obesity. Located on the fifth and seventh floors of the Hatfield building, the unit brings together experts from the fields of metabolism, endocrinology, nutrition, cardiovascular biology, gastroenterology, hepatology, genetics, and the behavioral sciences.
Obesity’s “connection to co-morbid conditions like diabetes, heart disease, and some forms of cancer will drive public health in the future,” NIH Director Dr. Elias Zerhouni said, adding that the CC is the ideal facility for multi-disciplinary research required to address the obesity epidemic. CC Director Dr. John I. Gallin said the unit exemplifies the CC’s concern for patients and patient care with an environment designed and furnished for the safety and comfort of patient volunteers participating in clinical research.
 |
|
Metabolic dietitian Merel Kozlosky (center, facing forward) gives a tour to (from left) Drs. Gallin, Gottesman, Skarulis, Zerhouni, and Rodgers.
|
According to Dr. Griffin Rodgers, acting director of NIDDK and co-chair of the NIH obesity research task force, the unit is an example of “syzygy,” a term often used to describe the alignment of celestial bodies, because so many disparate elements blended in the new space. Rodgers also called the unit a “trans-NIH effort” to act as an accelerator of understanding about the underpinnings of the nation’s obesity crisis.
Attendees at the open house had the opportunity to view an informational video produced by NIDDK describing the unit and its programs, as well as tour both floors and ask staff questions. Visiting staff also viewed a food array, a sampling of food items that allows investigators to observe what children and adults choose when presented with a buffet of food. The nutrition department will play a significant role in research conducted at the unit. A senior clinical research dietitian and a metabolic dietitian will be dedicated to the intra-institute obesity initiative. A metabolic health technician and metabolic cooks will also support this research.
The unit’s fifth floor includes 10 inpatient rooms, a metabolic kitchen, an exercise room, specialized vending machines, and a communal dining area. The design of each inpatient room on the unit took into account the needs of the patient volunteers, with specially reinforced construction, amenities, and equipment. The metabolic kitchen allows dietitians to precisely control the composition of patient diets and weigh items before and after a meal to calculate the exact nutrients consumed. “For many studies, we will also be collecting information about patients’ usual dietary patterns using food records and questionnaires,” said dietitian Nancy Sebring.
 |
|
Nancy Sebring, a clinical research dietitian, shows a photo of a sample food array to Dr. Gottesman.
|
The unit’s exercise testing equipment, physical activity monitors, body composition measurement tools, and three metabolic suites are key resources for clinical research protocols. The fitness equipment, including a treadmill and stationary upright and recumbent bikes, allows researchers to conduct stress and pulmonary function tests and other exercise interventions while the machines are in use to observe the effects of exercise on weight loss. The Bod Pod on the seventh floor measures total body density and lean and fat body mass using air—rather than the more typical water—displacement. The DXA scanner sweeps the entire body with a small-dose X-ray to calculate how much of the body is made up of fat, muscle, and bone. Unit staff also demonstrated the apnea risk evaluation system, a headpiece used in sleep studies to track measurements such as breathing, heart rate, oxygen saturation, head positioning, and snoring through a cannula inserted into the nose. Program equipment on both floors is regularly calibrated so that protocol-related physiological measurements are complete and precise.
Three rapid response respiratory suites on the seventh floor are the signature feature of the unit. They allow researchers to study a patient’s energy metabolism over 24 hours using non-invasive and comprehensive physiological measurements. By analyzing air composition in the suite, researchers will be able to determine how much energy on a minute-to-minute basis a volunteer burns while sleeping, eating, or exercising, and whether the energy comes from carbohydrate, protein, or fat. NIH staff custom-designed a vacuum-sealed porthole, or “isolette system,” through which measured food and blood samples can be passed so that physiological measurements are not disrupted. “People become obese or overweight because of small differences between calories taken in and calories expended over the long term,” said Dr. Monica Skarulis, a senior clinical investigator with NIDDK’s Clinical Endocrine Branch. “These metabolic suites will allow clinical researchers to collect precise and accurate measurements necessary to test new and innovative hypotheses about energy metabolism.” Dr. Kong Chen, director of the core laboratory on the unit, said the space will provide researchers with “unparalleled opportunities for new scientific discovery through cutting-edge clinical investigative, laboratory, and imaging capabilities.”
The unit, which is available to all institutes for obesity research, will open with protocols sponsored by several institutes including NIDDK and NICHD. The protocols will address how factors such as a person’s diet, exercise, or the amount of sleep he or she gets, combine with genetics to determine body weight. Skarulis said the unit seeks both obese and non-obese volunteers for protocols, “so everyone is welcome” to consider enrolling.
Back to Top
Social workers focus on hope, health
 |
|
Rolando Fuentes, a pediatric social worker, talks with patient Luana Veneziani. CC social workers provide services for patients and their families while they participate in trials here.
|
For the Social Work Department at the Clinical Center, “Hope and Health: Help Starts Here” is more than the theme of this March’s National Association of Social Workers’ national social work month. It’s a daily mandate. The 2007 theme highlights the important role of medical social workers in the well-being of hospital patients and their families. The nation’s 110,000 health-care social workers address more than physical needs. They take a holistic, psychosocial approach to provide the best overall care.
The CC Social Work Department, active since the hospital opened in 1953, provides critical services for patients, families, and staff—all in support of the CC’s research and clinical care mission. The department is a world leader in medical social work thanks to highly trained staff and innovative education, volunteer, language interpreting, human subjects protection, and HIV counseling programs.
 |
|
The department leads several monthly support group meetings for patients with conditions such as cancer and sickle cell anemia. Ihsan Rogers (left) leads a sickle cell support group meeting with (second from left) Zuleika Zapata; Clara Nsenkyire; her mother, Rose Nsenkyire; and Annie Brown.
|
Department Chief Dr. Adrienne Farrar said the department’s goal is to empower patients and families by providing counseling, health education, and community-referral services. “With a unique understanding of the diverse needs of research patients and families who come from all parts of the world, department staff have always maintained values of caring and expert service. We have a rich legacy as patient advocates and leaders in medical social work programs,” she said.
The department’s tradition of service and advocacy focuses on meeting the needs of patients and their families during extremely stressful and frightening situations. Staff also help with the practical issues of receiving medical care far from home. “Staff can assist with travel, lodging, and locating financial resources, from both within the NIH and in the community,” Farrar said. When patients are ready to return home, social workers often help locate resources in their community and help them coordinate care at home.
 |
|
The Social Work Department participates in interdisciplinary work, such as this weekly pain and palliative care meeting. Margo Aron (third from left), clinical social work program supervisor, meets with members of the team, which is made up of CC staff members from several departments and is led by the pain and palliative care services.
|
Margo Aron, clinical program supervisor, said the “most unique quality that we bring is to approach the patient from a more holistic perspective. We look at the whole patient: emotional, spiritual, social, family dynamics, and financial concerns— and how those impact on coping with illness.” In addition, “each patient, family, culture, and medical condition brings a different experience,” said social worker Patricia Prince. “The challenge we face is to assess each situation and bring the patient and caregivers together at the right time—to support both as needed.” Working with a diverse patient population is challenging, Prince said, but when life or death medical situations are involved, the cultural differences become even more complex. “The most rewarding part of my job is to work with patients who manage to thrive despite so many personal obstacles,” said Ihsan Rogers, a CC social worker for five years.
The Social Work Department promotes the mission of the CC through our contributions to the development and implementation of numerous initiatives including the Safra Family Lodge and The Children’s Inn,” Farrar said. “For more than 50 years department members have published, presented, and engaged in individual and collaborative research, both on a national and international level. Throughout our history, we have set a standard of quality and excellence in patient care.”
To honor the achievements of its staff and to illustrate the work performed by social workers, the CC Social Work Department will celebrate national social work month by hosting an open house on March 29 from 11 a.m. to 1 p.m. in their second-floor space, room 2-3581. All CC staff are invited to attend.
Back to Top
"Thanks, thanks, I give you thanks"
 |
Nicholas Clarke, at the Clinical Center since 2003, plays the 7th floor piano.
Job: patient messenger and escort, Ambulatory Care Services
|
If you’ve walked through the atrium in the afternoon, you may have heard faint piano music playing. If so, you’ve experienced the contribution of Nicholas Clarke, a messenger and escort with Ambulatory Care Services, to the unique environment in Building 10.
Clarke, who was born in Kingston, Jamaica, and came to the United States in October 2002, spends most of his day escorting patients to and from appointments in the CC and ferrying patient charts and specimens where they need to go. But during his half hour midday break, Clarke is usually at the piano. Clarke has never received formal piano lessons and can’t read music, but he loves to try to play whatever he hears. He doesn’t have a piano at home, so he values the practice time.
Often CC patients, staff, and physicians walking by or from the nearby clinics will approach Clarke to talk with him about his music. “It’s relaxing to them and most of the time they come up here to relax and listen,” he said. Clarke has never performed and would prefer to be in the background than a center-stage musician. He recalled volunteering to provide background music once when it was needed at a wedding he attended. “I’ll just go up and play if the keyboard is available,” he said.
Clarke’s favorite types of music to play are soul and gospel. He ends each practice session with the song, “Thanks, thanks, I give you thanks,” because “I always thank God for everything, for the gift of being able to play the piano and share it with people around me.”
Back to Top
Second couple celebrate 100 donations to NIH blood bank
 |
|
Mort and Sue Rudo celebrate their 100th blood bank donations.
|
When Sue Rudo made her 100th blood donation to the NIH blood bank, there was more to celebrate than just her milestone. Sue and her husband, Mort, became the second husband and wife team to each give blood here 100 times.
“Reaching 100 feels wonderful,” Sue said. “It’s a feeling of accomplishment,” added Mort, who made his 100th donation back in August of 2006. “Giving blood every eight weeks is also an incentive to stay healthy,” said Mort, a retired pharmacist. Sue is a retired executive secretary. They’ll be married 50 years in September. Not surprisingly, they told their donor story in tandem, finishing each others’ sentences as they explained how they started giving blood at the CC 20 years ago for a relative who was a patient.
“We felt very good about coming to NIH. It’s so professional and everyone treats us very well,” Mort said, adding, “We never thought of stopping. It became part of our lives.” Sue agreed that the process of donating blood is “really very easy. You just sort of get on a roll. Plus we got involved with the people here and looked forward to seeing them every eight weeks. We plan to continue giving.”
Sue admitted that for her there was an extra incentive: Her friend and former neighbor Barbara Norland, who also is in the 100-club at the blood bank, used to donate with Sue in the morning before work. They made it fun for each other by holding contests to see who would finish donating first, or who had the highest iron count.
The Rudos said they proudly tell people they are donors at NIH. As Sue explained, “When you stop and think how many people received our blood, how many people we’ve helped, it’s incredible.”
John and Elizabeth Diffley were the first couple to each make 100 blood donations. John achieved it in 2001 and Elizabeth in 1996. She was the first woman at the NIH Blood Bank to receive that recognition.
Back to Top
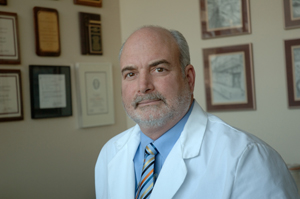
Captain Charles McGarvey retires from USPHS, CC after 30 years
|
|
Captain Charles McGarvey is recognized as an expert in the area of oncology in physical therapy.
|
Charles McGarvey, chief physical therapist in the physical therapy section of the Clinical Center’s Rehabilitation Medicine Department and Captain in the Commissioned Corps of the U.S. Public Health Service, retired from active service and the CC on Feb. 28. Commander Michaele Smith will serve as acting section chief and Captain Karen Siegel took over as chief professional officer for the Commissioned Corps' therapist category on Feb. 13.
During his career as a clinician, administrator, researcher, and educator, McGarvey focused on efforts to improve the quality of life of patients worldwide by creating and disseminating rehabilitation protocols for a wide range of illnesses, influencing the education of rehabilitation practitioners, and facilitating research focused on improving health outcomes. At NIH, McGarvey facilitated the development of standards of care in orthopedic, neurologic, cardiopulmonary, pediatric, and oncology rehabilitation and established criteria for evaluating and treating complex biomedical problems. Additionally, McGarvey created and tested techniques in pain assessment, electrophysiology, musculoskeletal screening, gait analysis, wound care, serial casting, and orthotic and prosthetic fabrication. Over the past 20 years, in the capacity of physical therapy section chief, McGarvey advanced and refined the role physical therapy plays in the interdisciplinary rehabilitation of functional challenges.
Clinically, McGarvey has worked almost exclusively with cancer patients for 18 years. Educationally, he has lectured extensively nationally and internationally on a variety of issues related to the assessment and treatment of cancer patients. In 1990, he published the text “Physical Therapy for the Cancer Patient” and has authored or co-authored more than 18 articles and chapters on cancer rehabilitation. From 1991 to 1992 he was selected by the Agency for Health Care Policy and Research to serve as the only physical therapist on two expert panels to develop nationally based guidelines for the assessment and treatment of acute post-operative pain and cancer pain. These guidelines served as the benchmark for the development and implementation of comprehensive pain management initiatives worldwide. In 1999, the National Naval Medical Center’s Breast Cancer Center invited McGarvey to develop and implement a program to provide comprehensive rehabilitation services to their population of patients with breast cancer. A major outcome of this program was the development and implementation of two NCI and NAVY-IRB approved protocols, for which McGarvey served as principal investigator.
Beginning in 1978, McGarvey presented more than 25 scientific papers and posters at state, national, and international conferences and meetings. McGarvey received 20 individual honor awards from USPHS and five honor awards from professional organizations, including the Jeri F. Walton Service Award for his contributions to oncology rehabilitation. The American Physical Therapy Association recently inducted him as a Catherine Worthingham fellow and he also received the Surgeon General’s exemplary service medal. After Hurricane Katrina as part of USPHS’ Team Alpha, McGarvey spent about a week in Baton Rouge, La., caring for evacuees in a makeshift hospital at Louisiana State University.
“I’m very grateful for the opportunity to work at NIH for the past 24 years,” McGarvey said. “I’m most proud of the performance of the physical therapy section and the advances in research and science that we as a group have contributed to the NIH and to our profession.” Smith said McGarvey has had “remarkable insight and vision to encourage his staff to embark on the next step of their careers. We will miss him greatly.”
McGarvey still will advise trials at NNMC and NIH. He also is starting a consulting service.
Back to Top
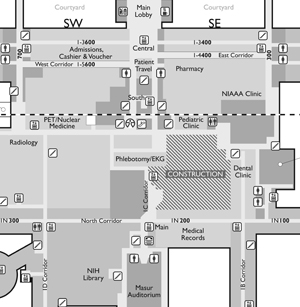
Construction scheduled on Magnuson building first floor
|
|
|
Work during the first phase of construction projects in the Magnuson building will affect areas around the old VIC.
|
A collection of construction projects slated to begin in late March will provide renovated space for several Clinical Center programs and create a new central, straight-shot corridor connecting the first floor of the Hatfield building (near the escalators) to Masur Auditorium by late 2008.
Work will be conducted in three phases. During Phase 1, construction barricades will block the familiar diagonal corridor that connects the Magnuson building’s N (for North) corridor to the main elevators near Masur Auditorium. Also blocked will be the ramp adjacent to the now-closed Visitors Information Center (VIC), along with open areas in the 2nd floor cafeteria that overlook the VIC.
Access to the dental clinic will remain open, as will all offices along the corridor that connects Lipsett Amphitheater and Diagnostic Radiology.
Also during Phase 1, the DCRI Information Technology Center, conference room, and some offices will relocate to renovated space near the main elevators on B1.
New signage will redirect traffic to an existing north-south hallway adjacent to DCRI and radiology. This will serve as the main connector between the Hatfield and Magnuson buildings for the duration of Phase 1, approximately four months.
During Phase 2, expected to last about 12 months beginning in late summer, planned construction includes new facilities for pharmacy functions, primarily pharmaceutical production. Those facilities, and some offices, were not relocated to the Hatfield building when it opened in 2004. Pharmacy work will be in the area between the North corridor, the dental clinic, the VIC, and the temporary north-south corridor. New space for phlebotomy/EKG will be constructed next to their current location.
Highlights of the project’s third and final phase include opening the new Hatfield-Magnuson central corridor and construction of a new corridor on B2. Connecting the loading dock to the west end of the CC, the corridor will be used by small trucks called “tuggers,” which currently share hallways with pedestrians, transport materials, and supplies.
While the cavernous VIC will remain behind construction barricades during all phases, no construction or renovation on the space is scheduled for at least 12 months.
Back to Top
Installation of glass plates in atrium begins
|

|
|
A worker begins installing glass panels above the railings that ring the atrium of the Hatfield building.
|
Another construction project is in progress in the Hatfield building—installation of glass panels above the railings that ring the atrium. Two floors will be affected at a time. The work, including construction of safety barriers, will be completed first on each floor’s west side, then on the east.
As part of the project, steel mesh will be installed between the top of the existing glass and the ceiling on the seventh floor. Throughout the work, which is expected to be complete in mid-summer, safety barriers will remain in place on the first floor.
Back to Top
Honor MLK, give help
 |
|
CC Director Dr. John I. Gallin and NIH Director Dr. Elias Zerhouni present Dr. LaSalle D. Laffall, Jr., (center) with a poster commemorating his keynote address for the annual program honoring Dr. Martin Luther King, Jr., on Jan. 18.
|
Leffall is the Charles R. Drew professor of surgery at Howard University College of Medicine and chair of the President’s Cancer Panel, Susan G. Komen for the Cure, and C-Change. In his statements, Leffall applied Dr. King’s concept of a network of human mutuality to the CC’s work, which he said lives out what Dr. King considered to be man’s ultimate gift: to see someone in need and give help. “It’s not just that you live, but how you live,” Leffall said.
Back to Top
Valentine's Day party sweetens life at CC
The recreational therapy section’s Valentine’s Day party on Feb. 8 offered patients, their families, and staff the opportunity to enjoy crafts and community in celebration of the holiday.
Several volunteers assisted CC staff in setting up and serving refreshments to party goers.
 |
|
CC patient Eric Petel and his mother, Helen, paint pottery with a Valentine’s Day theme.
|
|

|
Elvera Sales, a staff member with the recreational therapy section, melts pieces of milk, white, and pink chocolate to be molded into heart-shaped lollipops
|
Back to Top
News Briefs
Learn about health information privacy and security April 9-13
As the health-care industry moves closer to electronic health information systems, privacy concerns remain an important issue. Please join the CC’s medical record department in raising awareness among health-care professionals and the public on the importance of protecting the privacy, confidentiality, and security of health information. Look for information tables throughout the week.
Hospital epidemiology moves
On Feb. 14, the CC Hospital Epidemiology Service moved from 10S239 to 2N224. Located in a well-traveled area on the north side of the second floor near the Magnuson Center’s main elevators, the new space will be more visible and accessible to staff, who are encouraged to drop in with their infection control concerns.
Two communications staffers relocate
Jenny Haliski and Shana Potash, who handle CC News and media relations for the Office of Clinical Center Communications, are now located in 2C202, across from the cafeteria.
Correction
While visiting the CC on Jan. 17, President Bush met with patients, families, and staff and participated in a roundtable discussion on advances in cancer prevention on 3NW, not 3SW.
Back to Top
Research volunteers needed for studies
Neck pain study
Volunteers with or without neck pain ages 18 to 65 needed to participate in a three-month natural history study (02-CC-0245) involving four one-hour visits. Contact at neckpainstudy@gmail.com, 301-496-4733.
To participate in any of the following studies, call 1-866-444-2214 or
TTY: 1-866-411-1010.
ADHD genetics study
Volunteers needed for a study (00-HG-0058) seeking to identify the genes that contribute to attention deficit hyperactivity disorder.
Gingival overgrowth study
Patients with enlarged gums using dilantin, cyclosporine, or calcium channel-blockers needed for a study (05-D-0103).
Osteoarthritis study
Men ages 30 to 65 needed for a study (04-AT-0239) evaluating hormones. Compensation provided.
Ovarian function study
Women ages 18 to 25 needed for an ovarian function study (00-CH-0189).
Back to Top
New clinical research protocols
The following new clinical research protocols were approved in January:
A Feasibility Study to Test an Individualized Dyadic Problem-Solving Education Intervention to Improve Problem-Solving Skills of Patients and Family Caregivers During Allogeneic HSCT, 07-CC-0067, Margaret F. Bevans, PhD, CC
Prospective Evaluation of Tumor Angiogenesis in Endocrine Neoplasms, 07-C-0060, Steven K. Libutti, MD, NCI
Phase II Study of Clinical Activity and Proteomic Pathway Profiling of the VEGFR2 Inhibitor, Vandetanib in Women With Relapsed or Refractory Epithelial Ovarian, Fallopian Tube, or Primary Peritoneal Cancer, 07-C-0061, Elise C. Kohn, MD, NCI
A Phase II Study of AZD2171 in Metastatic Androgen Independent Prostate Cancer, 07-C-0059, William L. Dahut, MD, NCI
Adoptive Cell Therapy for B-Cell Malignancies After Allogeneic Hematopoietic Stem Cell Transplantation with Costimulated, Tumor-Derived Lymphocytes, 07-C-0064, Michael R. Bishop, MD, NCI
Double-Blind, Randomized Controlled Trial of Voriconazole Plus Micafungin Versus Voriconazole Plus Placebo in the Treatment of Patients with Proven or Probable Invasive Aspergillosis, 07-C-0071, Thomas J. Walsh, MD, NCI
A Phase II Study of ABT-751, an Orally Bioavailable Tubulin Binding Agent, in Children with Relapsed or Refractory Neuroblastoma, 07-C-0074, Elizabeth Fox, MD, NCI
A Phase I/II Study of Flavopiridol in Relapsed or Refractory Mantle Cell Lymphoma (MCI) and Diffuse Large B-Cell Lymphoma (DLBCL), 07-C-0081, Kieron M. Dunleavy, MD, NCI
An Exploratory Study of the Use of Five Wishes as a Tool for Advanced Care Planning in Young Adults with Metastatic, Recurrent, or Progressive Cancer, 07-C-0085, Lori Wiener, PhD, NCI
Pilot Study of Educational Interventions in Pediatric Hematopoietic Stem Cell Donors to Increase Knowledge of Donation and Transplantation Procedures, 07-C-0086, Lori Wiener, PhD, NCI
Modifying Tolerance to Ischemic Injury in Human Atrial Tissue, 07-H-0057, Michael Sack, MD, NHLBI
Allogeneic and Matched Unrelated Donor Stem Cell Transplantation for Congenital Immunodeficiencies: Busulfan-Based Conditioning with Campath-1H, Radiation, and Sirolimus, 07-I-0075, Elizabeth M. Kang, MD, NIAID
Phase I Study of the Safety and Immunogenicity of AMA1-C1/Alhydrogel + CPG 7909, an Asexual Blood Stage Vaccine for Plasmodium Falciparum Malaria, 07-I-0083, Ruth D. Ellis, MD, NIAID
Study of the Phenotype of Overweight and Obese Adults, 07-DK-0077, Monica C. Skarulis, MD, NIDDK
Belatacept Evaluation of Nephroprotection and Efficacy as First Line Immunosuppression Trial (BENEFIT), 07-DK-0070, Allan D. Kirk, MD, NIDDK
Detecting a Reward Signal in the Motor Cortex, 07-N-0063, Eric M. Wassermann, MD, NINDS
Direct Current Brain Polarization of Bilateral Prefrontal Cortex, 07-N-0066, Eric M. Wassermann, MD, NINDS
Neural Substrates of Lasting Motor Skill Learning by Spacing Effect, 07-N-0072, Leonardo G. Cohen, MD, NINDS
Back to Top
Upcoming Events
Clinical Center Grand Rounds and Great Teachers Lectures
March 7, 2007
Hormones and Epilepsy: How Menstruation, Stress, and Hypogonadism Influence Seizure Susceptibility
Michael A. Rogawski, M.D., Ph.D.
Professor and Chair, Department of Neurology, University of California, Davis
Kennedy’s Disease
Kenneth Fischbeck, M.D.
Chief, Neurogenetics Branch, NINDS
March 14, 2007
Great Teachers
Contemporary Clinical Medicine: Great Teachers
Translation, Replication, and Credibility of Research Findings
John P. A. Ioannidis, M.D., Ph.D.
Professor and Chairman, Department of Hygiene and Epidemiology
University of Ioannina School of Medicine, Ioannina, Greece
March 21, 2007
The Pathophysiology of Bone Marrow Failure
Neal Young, M.D.
Chief, Hematology Branch, NHLBI
Advances in the Treatment of Aplastic Anemia
Phillip Scheinberg, M.D.
Staff Clinician, Hematology Branch, NHLBI
March 28, 2007
Depression, Anxiety, and Alcoholism: What is the Link? Lessons From Epidemiology and Neurobiology
Bridget F. Grant, Ph.D., Ph.D.
Chief, Laboratory of Epidemiology and Biometry, Division of Intramural Clinical and Biological Research, NIAAA
Markus Heilig, M.D., Ph.D.
Clinical Director; Chief, Laboratory of Clinical and Translational Studies, NIAAA
Back to Top
Clinical Center News, National
Institutes of Health, Building 10, 10 Center Drive, Room 12C440, Bethesda, MD 20892-1504. Tel: 301-496-6787.
Fax: 301-402-2984. Published monthly for CC employees
by the Office of Communications, Patient Recruitment, and Public Liaison. News, article ideas,
calendar events, letters, and photographs are welcome.
Back to Top
|
|


 The information on this page is archived and provided for reference purposes only.
The information on this page is archived and provided for reference purposes only.